Daily Quizzes
Mock Tests
No tests attempted yet.
Select Category

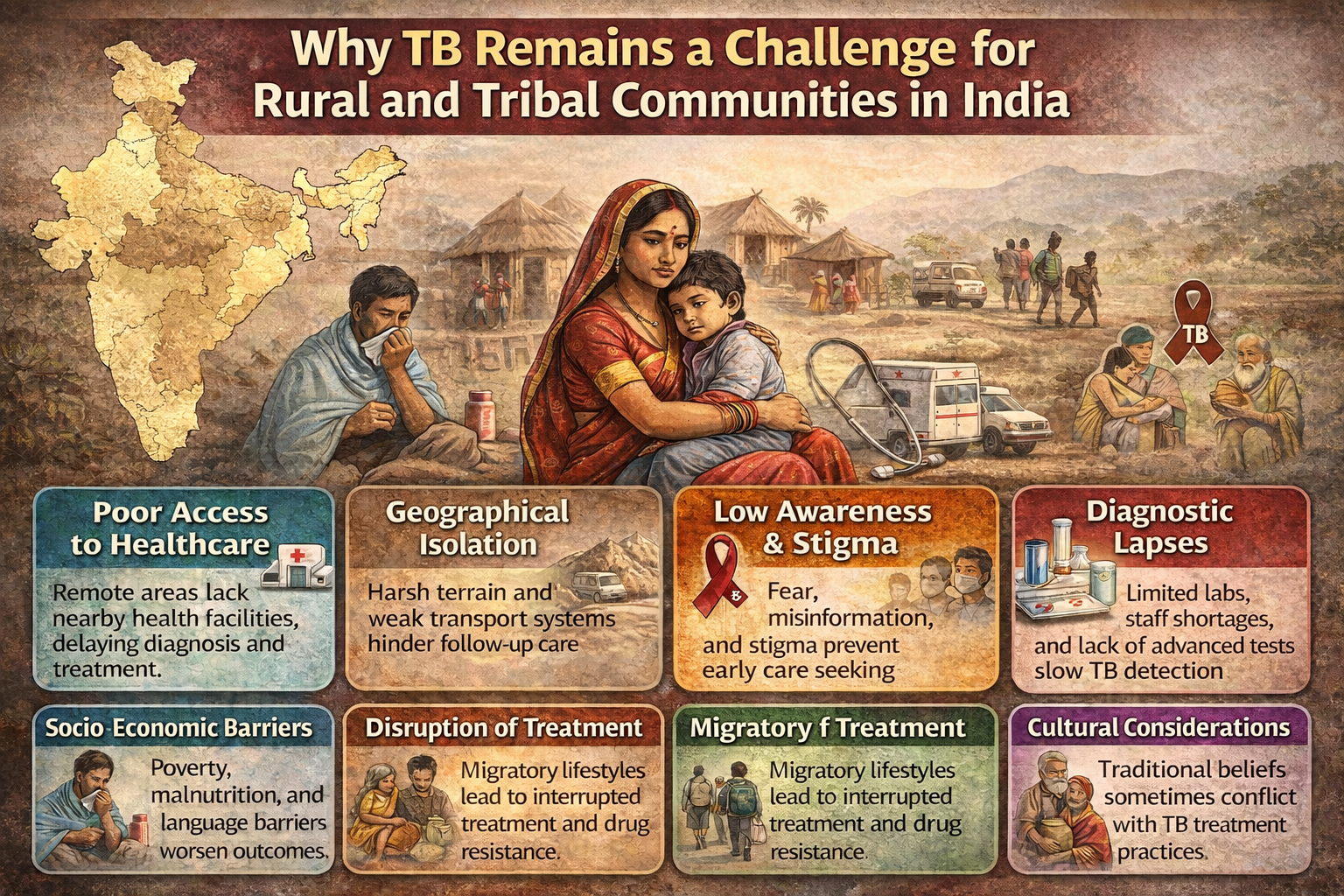
Tuberculosis is a significant social and human health issue in India and other countries and is disproportionately affecting rural, tribal and migrant populations who have an overview of obstacles. Such populations tend to reside in rural or underserved regions and have poor access to medical care, diagnostic services and follow-up treatment. Geographic isolation, poverty, cultural and language barriers, stigma, and poor health infrastructure postpone the diagnosis and treatment of TB, making it more vulnerable and spreading the disease. Migrants specifically face interrupted treatment as a result of mobility and poor living conditions, and tribal populations are subject to institutional unfairness and social exclusion that obstructs the control of TB. These are the combined problems that need tackling to achieve the elimination targets.
Why TB Remains a Challenge for Rural and Tribal Communities in India
-
Poor access to healthcare: Isolated rural and tribal areas may have no health facilities nearby, meaning people have to travel long distances to obtain a diagnosis and treatment.
-
Geographical isolation: Harsh terrain and poor transport infrastructure prevent timely access to healthcare and follow-up.
-
Low awareness/stigma: Some people are unaware of TB, and stigma prevents early care-seeking.
-
Diagnostic lapses: Poor laboratory facilities, staff shortages, and the unavailability of high-tech tests slow case detection.
-
Socio-economic barriers: Poverty, malnutrition, and language barriers worsen outcomes in these populations.
-
Disruption of treatment: TB treatment adherence is difficult due to a migratory lifestyle and the absence of continuous care.
-
Cultural considerations: Cultural beliefs are at odds with modern TB treatment methods.
PYQs Questions Based on TB
| Exam | Year | Question | Answer |
|---|---|---|---|
| Rajasthan CET (Senior Secondary) | 2023 | The Government of India has fixed the goal to achieve TB Free India by _______. | 2025 |
| NHM MP CHO Official Paper | 2022 | Tuberculosis surveillance system called “_______” for both govt and private health facilities. | Ni-kshay |
| MPPSC General Aptitude | 2018 | Statement: Tuberculosis (TB) is a pandemic issue now. Which assumption is strong? I) The Govt should work to eradicate diseases like polio. II) TB is not serious, and treatment is available. |
Assumption I is strong |
| UPSC Daily Current Affairs (Mock Question) | 2021 | Regarding Tuberculosis: It is caused by bacteria and spread by mosquitoes; it’s preventable & treatable. Which are correct? | 1 and 3 only (caused by bacteria & preventable/curable) |
| UPSC Prelims Test | 2016 | Statements: 1) TB is caused by a virus spread by air 2) BCG vaccination prevents severe forms in children 3) MDR-TB is resistant to isoniazid & rifampin Which are correct? |
2 and 3 |
Important Expected Questions
Which of the following is the correct causative agent of tuberculosis (TB)?
a) Virus
b) Bacteria
c) Fungus
d) Protozoa
Answer: b) Bacteria
Explanation: TB is caused by Mycobacterium tuberculosis, a bacterium that primarily affects the lungs but can involve other organs.
What is the purpose of the “Ni‑kshay” portal in India?
a) To track TB patients
b) To provide free vaccines
c) To distribute nutritional supplements
d) To report malaria cases
Answer: a) To track TB patients
Explanation: Ni‑kshay is a government portal used for TB surveillance, patient management, and ensuring treatment adherence.
Which vaccine is given to prevent severe forms of TB in children?
a) DPT
b) BCG
c) MMR
d) Polio
Answer: b) BCG
Explanation: The BCG (Bacillus Calmette–Guérin) vaccine helps protect children against severe TB forms like TB meningitis.
MDR-TB refers to:
a) TB resistant to only one drug
b) TB resistant to isoniazid and rifampin
c) TB cured naturally without medicine
d) Drug-sensitive TB
Answer: b) TB resistant to isoniazid and rifampin
Explanation: Multi-Drug Resistant TB (MDR-TB) occurs when TB bacteria resist the two most effective first-line drugs.
Why are rural and tribal communities more vulnerable to TB?
a) Poor healthcare access
b) Poverty and malnutrition
c) Low awareness and stigma
d) All of the above
Answer: d) All of the above
Explanation: Multiple factors—geographical, socio-economic, and cultural—make TB control challenging in these populations.
Conclusion (Challenges Aplenty for Rural Groups in Fighting TB)
The rural, tribal and migrant populations still have a huge burden to overcome TB due to lack of healthcare, geographical isolation, poverty, poor awareness and social stigmas. To minimize TB burden and reach the elimination objective, it is necessary to strengthen healthcare infrastructure, increase awareness, ensure treatment adherence, and create special government programmes


 National Science Day 2026: Honouring C. V. Raman's Legacy of Discovery
National Science Day 2026: Honouring C. V. Raman's Legacy of Discovery PM Modi Reaffirms India’s Strong Support for Israel in Knesset Address
PM Modi Reaffirms India’s Strong Support for Israel in Knesset Address Supreme Court’s Suo Motu Case on NCERT Judicial Corruption Row
Supreme Court’s Suo Motu Case on NCERT Judicial Corruption Row Sachin Tendulkar Becomes UN Global Champion for Road Safety
Sachin Tendulkar Becomes UN Global Champion for Road Safety Punjab Launches ‘Meri Rasoi’ Scheme
Punjab Launches ‘Meri Rasoi’ Scheme Kerala Cabinet Approves Nativity Card Bill to Provide Permanent Proof of State Origin
Kerala Cabinet Approves Nativity Card Bill to Provide Permanent Proof of State Origin Prince Andrew’s Arrest Revives Jeffrey Epstein Scandal, Global Pressure Mounts
Prince Andrew’s Arrest Revives Jeffrey Epstein Scandal, Global Pressure Mounts PM RAHAT Scheme
PM RAHAT Scheme PM Modi and Macron to Launch India-France Year of Innovation 2026
PM Modi and Macron to Launch India-France Year of Innovation 2026 Great Nicobar Project approved by NGT
Great Nicobar Project approved by NGT