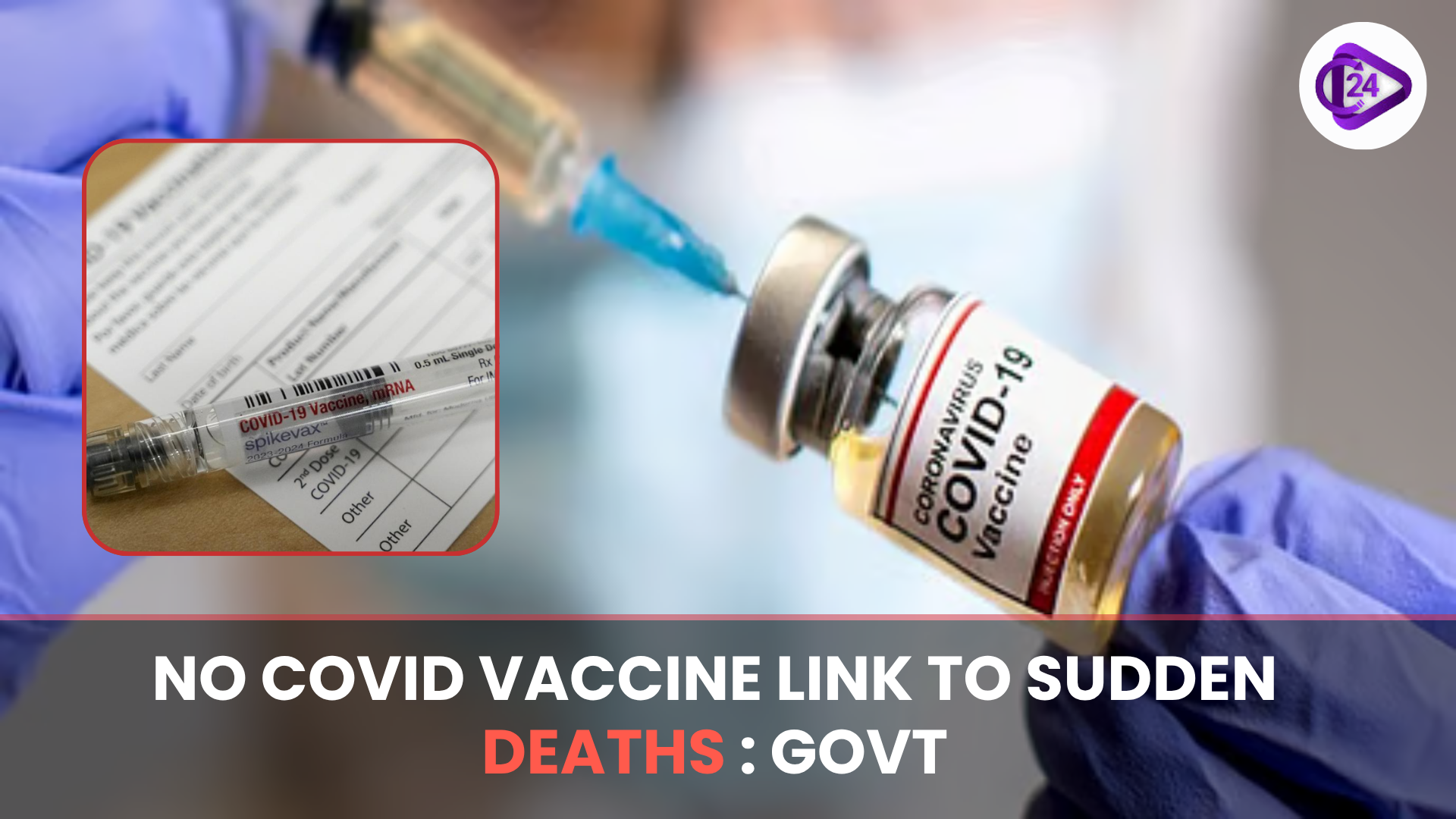
According to the Union Health Ministry, COVID-19 vaccines do not augment the risk of sudden unexplained death, particularly among young adults. This is an elaboration that has been done by the ICMR and the NCDC following stringent research studies. Such research has compared how death rates occur throughout India since the vaccination and have discovered that there was no statistically significant difference in comparison with earlier years. It was identified that more likely causes are genetic factors, lifestyles, as well as post-COVID complications. The Ministry cautioned against the use of misinformation, which is likely to increase vaccine hesitancy.
Context
-
The scientific investigation has not revealed any causal relationship between sudden deaths amid young adults in India and COVID-19 vaccines.
-
The Health Ministry pointed out that there exists falseness on this matter and which is not scientifically based.
Key Points
Investigating Agencies
-
ICMR (Indian council of medical research)
-
National Centre of Disease Control (NCDC)
-
AIIMS (in ongoing study) (All India Institute of Medical Sciences)
Important Research and Results
Study 1:
-
Title: Factors related to unexplained sudden mortality among individuals aged 18 45 years in The Indian subcontinent
-
Study design: Retrospective matched case control study
-
Done by: ICMR-NIE
-
Dates: May June July 2023
-
Geographical Divisions: 19 states/UTs and 47 tertiary care hospitals
-
The finding is that there is no association between sudden deaths and COVID-19 vaccines.
Study 2:
-
Title: “Establishing the cause in sudden unexplained deaths in young”
-
Type: Prospective study
-
Performed by: AIIMS (with collaboration of ICMR)
-
Initial Grasping: The most frequent cause of sudden death among the adult population is a heart attack (myocardial infarction)
Reasons found behind the sudden deaths
-
Genetic predispositions
-
Harmful recreational activities (e.g. smoking, drug abuse, stress)
-
Pre Existing conditions (e.g. untreated condition of the heart)
-
Post-COVID-19 complications
Government’s Stand
-
Against faith in the safety of vaccines
-
Misinformation can result in vaccine terrorization, which should be warned.
-
Highlighted the life-saving quality of vaccines against the pandemic
About vaccine misinformation
What is Vaccine misinformation?
-
intentionally or unintentionally inaccurate or misleading information regarding vaccines. It has proved to be a tremendous challenge to public health policy especially in health emergencies such as the COVID-19 pandemic.
How Vaccine Misinformation Affects Public Health Policy
1. Vaccine Hesitancy
-
Definition: Refusal or acceptance delay of vaccines even when available.
-
Effect: Decreases the coverage of vaccination opening up the potential of losses to herd immunity.
-
Example: India: Rumours of infertility induced by COVID-19 vaccine vaccines led to suspicion in the rural areas.
2. Healthcare Systems Pressure
-
The false information results in reduced vaccination rates, which predisposes people to greater promotion of the disease.
-
Increased hospitalization and number of admissions into ICUs strain an already overextended public health infrastructure.
3. Erosion of public trust
-
Confidence in science, experts and institutions is compromised.
-
Makes future health ones harder to deal with (e.g. booster shots, campaign to immunize children).
4. Policy Redirection
-
Governments might have to reserve budget towards counter-misinformation initiatives at the expense of the primary health facilities.
-
Mismanagement of universal immunization programmes such as Mission Indradhanush.
5. International Ramifications
-
Influences international traveling regulations and vaccine export (since the lack of faith in vaccines may cause coverage imbalances).
-
The low vaccine-confidence countries could be restricted to various degrees or dealt with limited organization in international health arenas.
6. Legal and ethical Dilemmas
-
The controversy is about compulsory vaccination, freedom of speech or the safety of the masses.
-
Falsehood makes policy making about the use of coercion vs. persuasion on vaccine outreach hard to come by.
Creating Strategies to Counter Vaccine Misinformation
-
Citizen Education Programs
-
Through the involvement of community leaders, influencers and local media.
-
Ex. The Har Ghar Dastak campaign of India.
-
-
Regulation and Fact-Checking
-
Collaborations, such as with Twitter, WhatsApp, YouTube users are used to report or delete misinformation.
-
Promoting reliable scientific websites by government sites.
-
-
Legal Frameworks
-
Penalizing deliberate misinformation using law such as the Information Technology Act, Disaster Management Act or the Epidemic Diseases Act.
-
-
Civil Society interaction
-
Working with NGOs, health workers, ASHA workers to give grassroots information.
-
Conclusion
The evidenced-based stand of the Indian government has shown that there was no relevance between COVID-19 vaccines and sudden deaths among young adults. This increases the confidence of the people in scientific procedures and the relevance of evidence-based health communication in addressing misinformation.


 Phone Tapping Not Permissible for Crime Detection: Madras High Court
Phone Tapping Not Permissible for Crime Detection: Madras High Court Indian Railways Launches RailOne Super App to Simplify Passenger Services
Indian Railways Launches RailOne Super App to Simplify Passenger Services INS Tamal, Last Foreign-Built Navy Ship, Commissioned
INS Tamal, Last Foreign-Built Navy Ship, Commissioned Understanding Hul Diwas: The Legacy of the Santhal Rebellion
Understanding Hul Diwas: The Legacy of the Santhal Rebellion India’s Secular Constitution, Even Without the Word
India’s Secular Constitution, Even Without the Word India Adds 683 New Fauna Species and 433 Flora Taxa in 2024
India Adds 683 New Fauna Species and 433 Flora Taxa in 2024 52 Villages Along LAC and LoC in Ladakh to Get Reservation Benefits
52 Villages Along LAC and LoC in Ladakh to Get Reservation Benefits India Puts a ban to Jute Imports by Bangladesh through Land and Sea Ports
India Puts a ban to Jute Imports by Bangladesh through Land and Sea Ports Bid to Snatch Control of Tansen’s Tomb: Repeated Legal Challenges Over 16th Century Monument
Bid to Snatch Control of Tansen’s Tomb: Repeated Legal Challenges Over 16th Century Monument